ARI HCP ISI
Important Safety Information for ARISTADA HCP Website
- Indication Section
-
INDICATION
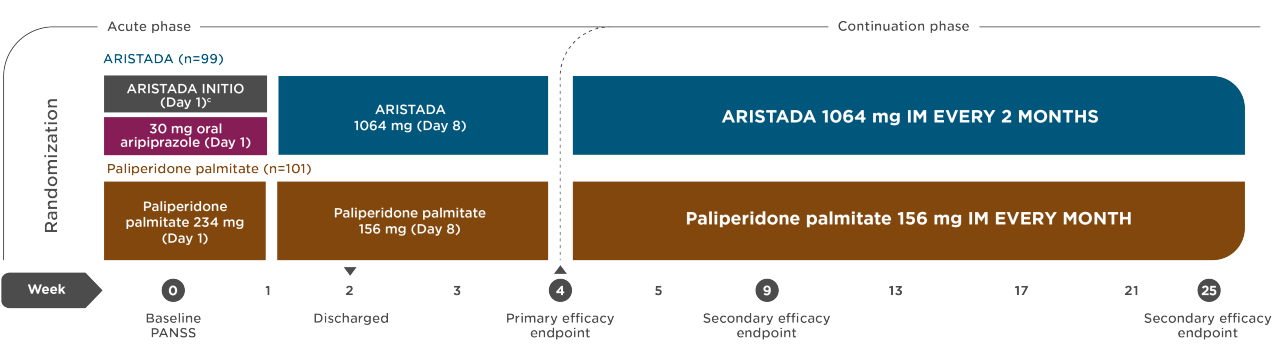
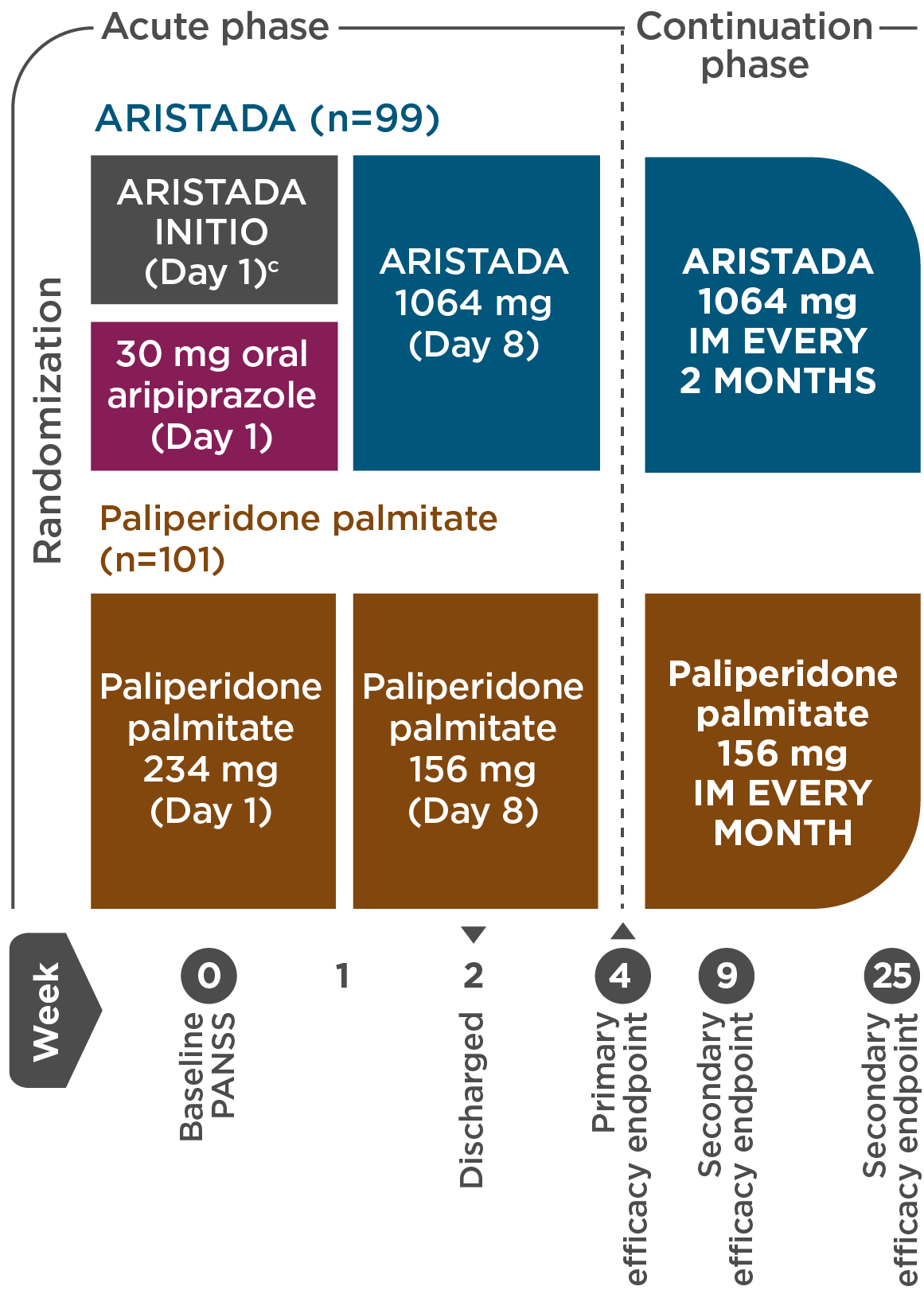
ARISTADA INITIO® (aripiprazole lauroxil), in combination with oral aripiprazole, is indicated for the initiation of ARISTADA® (aripiprazole lauroxil) when used for the treatment of schizophrenia in adults.
ARISTADA is indicated for the treatment of schizophrenia in adults.
- ISI Section Title
-
IMPORTANT SAFETY INFORMATION
- Boxed Warning
-
BOXED WARNING: INCREASED MORTALITY IN ELDERLY PATIENTS WITH DEMENTIA-RELATED PSYCHOSIS
Elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death. ARISTADA INITIO and ARISTADA are not approved for the treatment of patients with dementia-related psychosis.
- ISI Copy
-
Contraindication: Known hypersensitivity reaction to aripiprazole. Reactions have ranged from pruritus/urticaria to anaphylaxis.
Cerebrovascular Adverse Reactions, Including Stroke: Increased incidence of cerebrovascular adverse reactions (e.g., stroke, transient ischemic attack), including fatalities, have been reported in placebo-controlled trials of elderly patients with dementia-related psychosis treated with risperidone, aripiprazole, and olanzapine. ARISTADA INITIO and ARISTADA are not approved for the treatment of patients with dementia-related psychosis.
Potential for Dosing and Medication Errors: Medication errors, including substitution and dispensing errors, between ARISTADA INITIO and ARISTADA could occur. ARISTADA INITIO is intended for single administration in contrast to ARISTADA which is administered monthly, every 6 weeks, or every 8 weeks. Do not substitute ARISTADA INITIO for ARISTADA because of differing pharmacokinetic profiles.
Neuroleptic Malignant Syndrome (NMS): A potentially fatal symptom complex may occur with administration of antipsychotic drugs, including ARISTADA INITIO and ARISTADA. Clinical manifestations of NMS include hyperpyrexia, muscle rigidity, altered mental status, and evidence of autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis, and cardiac dysrhythmia). Additional signs may include elevated creatine phosphokinase, myoglobinuria (rhabdomyolysis), and acute renal failure. The management of NMS should include: 1) immediate discontinuation of antipsychotic drugs and other drugs not essential to concurrent therapy; 2) intensive symptomatic treatment and medical monitoring; and 3) treatment of any concomitant serious medical problems for which specific treatments are available.
Tardive Dyskinesia (TD): The risk of developing TD (a syndrome of abnormal, involuntary movements) and the potential for it to become irreversible are believed to increase as the duration of treatment and the total cumulative dose of antipsychotic increase. The syndrome can develop, although much less commonly, after relatively brief treatment periods at low doses. Prescribing antipsychotics should be consistent with the need to minimize TD. Discontinue ARISTADA if clinically appropriate. TD may remit, partially or completely, if antipsychotic treatment is withdrawn.
Metabolic Changes: Atypical antipsychotic drugs have been associated with metabolic changes that include:
- Hyperglycemia/Diabetes Mellitus: Hyperglycemia, in some cases extreme and associated with ketoacidosis, coma, or death, has been reported in patients treated with atypical antipsychotics. There have been reports of hyperglycemia in patients treated with oral aripiprazole. Patients with diabetes should be regularly monitored for worsening of glucose control; those with risk factors for diabetes should undergo baseline and periodic fasting blood glucose testing. Any patient treated with atypical antipsychotics should be monitored for symptoms of hyperglycemia, including polydipsia, polyuria, polyphagia, and weakness. Patients who develop symptoms of hyperglycemia should also undergo fasting blood glucose testing. In some cases, hyperglycemia has resolved when the atypical antipsychotic was discontinued; however, some patients require continuation of antidiabetic treatment despite discontinuation of the suspect drug.
- Dyslipidemia: Undesirable alterations in lipids have been observed in patients treated with atypical antipsychotics.
- Weight Gain: Weight gain has been observed with atypical antipsychotic use. Clinical monitoring of weight is recommended.
Pathological Gambling and Other Compulsive Behaviors: Compulsive or uncontrollable urges to gamble have been reported with use of aripiprazole. Other compulsive urges less frequently reported include sexual urges, shopping, binge eating and other impulsive or compulsive behaviors which may result in harm for the patient and others if not recognized. Closely monitor patients and consider dose reduction or stopping aripiprazole if a patient develops such urges.
Orthostatic Hypotension: Aripiprazole may cause orthostatic hypotension which can be associated with dizziness, lightheadedness, and tachycardia. Monitor heart rate and blood pressure, and warn patients with known cardiovascular or cerebrovascular disease and risk of dehydration and syncope.
Falls: Antipsychotics including ARISTADA INITIO and ARISTADA may cause somnolence, postural hypotension or motor and sensory instability which may lead to falls and subsequent injury. Upon initiating treatment and recurrently, complete fall risk assessments as appropriate.
Leukopenia, Neutropenia, and Agranulocytosis: Leukopenia, neutropenia and agranulocytosis have been reported with antipsychotics. Monitor complete blood count in patients with pre-existing low white blood cell count (WBC)/absolute neutrophil count or history of drug-induced leukopenia/neutropenia. Discontinue ARISTADA INITIO and/or ARISTADA at the first sign of a clinically significant decline in WBC and in severely neutropenic patients.
Seizures: Use with caution in patients with a history of seizures or with conditions that lower the seizure threshold.
Potential for Cognitive and Motor Impairment: ARISTADA INITIO and ARISTADA may impair judgment, thinking, or motor skills. Patients should be cautioned about operating hazardous machinery, including automobiles, until they are certain therapy with ARISTADA INITIO and/or ARISTADA does not affect them adversely.
Body Temperature Regulation: Disruption of the body’s ability to reduce core body temperature has been attributed to antipsychotic agents. Advise patients regarding appropriate care in avoiding overheating and dehydration. Appropriate care is advised for patients who may exercise strenuously, may be exposed to extreme heat, receive concomitant medication with anticholinergic activity, or are subject to dehydration.
Dysphagia: Esophageal dysmotility and aspiration have been associated with antipsychotic drug use; use caution in patients at risk for aspiration pneumonia.
Concomitant Medication: ARISTADA INITIO is only available at a single strength as a single-dose pre-filled syringe, so dosage adjustments are not possible. Avoid use in patients who are known CYP2D6 poor metabolizers or taking strong CYP3A4 inhibitors, strong CYP2D6 inhibitors, or strong CYP3A4 inducers, antihypertensive drugs or benzodiazepines.
Depending on the ARISTADA dose, adjustments may be recommended if patients are 1) known as CYP2D6 poor metabolizers and/or 2) taking strong CYP3A4 inhibitors, strong CYP2D6 inhibitors, or strong CYP3A4 inducers for greater than 2 weeks. Avoid use of ARISTADA 662 mg, 882 mg, or 1064 mg for patients taking both strong CYP3A4 inhibitors and strong CYP2D6 inhibitors. (See Table 4 in the ARISTADA full Prescribing Information.)
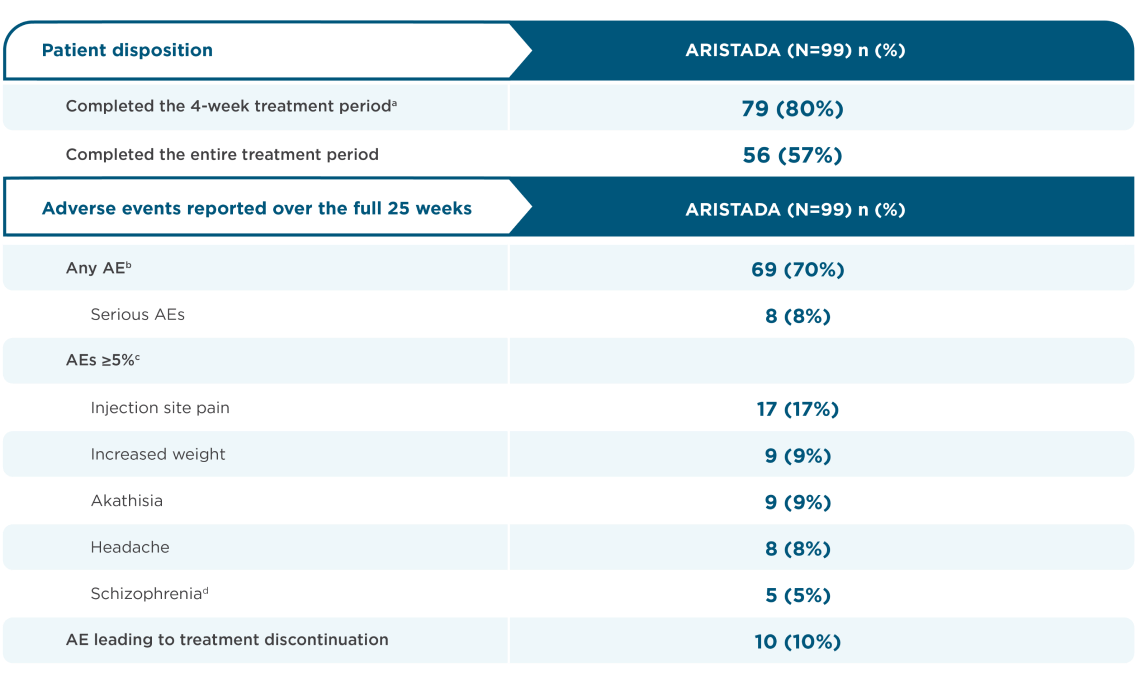
Commonly Observed Adverse Reactions: In pharmacokinetic studies the safety profile of ARISTADA INITIO was generally consistent with that observed for ARISTADA. The most common adverse reaction (≥5% incidence and at least twice the rate of placebo reported by patients treated with ARISTADA 441 mg and 882 mg monthly) was akathisia.
Injection Site Reactions: In pharmacokinetic studies evaluating ARISTADA INITIO, the incidences of injection site reactions with ARISTADA INITIO were similar to the incidence observed with ARISTADA. Injection site reactions were reported by 4%, 5%, and 2% of patients treated with 441 mg ARISTADA (monthly), 882 mg ARISTADA (monthly), and placebo, respectively. Most of these were injection site pain and associated with the first injection and decreased with each subsequent injection. Other injection site reactions (induration, swelling, and redness) occurred at less than 1%.
Dystonia: Symptoms of dystonia, prolonged abnormal contractions of muscle groups, may occur in susceptible individuals during the first days of treatment and at low doses.
Pregnancy/Nursing: Neonates exposed to antipsychotic drugs, including ARISTADA INITIO and ARISTADA, during the third trimester of pregnancy are at risk for extrapyramidal and/or withdrawal symptoms. Advise patients to notify their healthcare provider of a known or suspected pregnancy. Inform patients that there is a pregnancy exposure registry that monitors pregnancy outcomes in women exposed to ARISTADA INITIO and/or ARISTADA during pregnancy. Aripiprazole is present in human breast milk. Aripiprazole exposure during pregnancy and/or the postpartum period may decrease milk supply. Monitor the breastfed infant for dehydration and lack of appropriate weight gain. The benefits of breastfeeding should be considered along with the mother’s clinical need for ARISTADA INITIO and/or ARISTADA and any potential adverse effects on the infant from ARISTADA INITIO and/or ARISTADA or from the underlying maternal condition.
To report SUSPECTED ADVERSE REACTIONS, contact Alkermes at 1-866-274-7823 or FDA at 1-800-FDA-1088
or https://www.fda.gov/medwatch. - Prescription Information
-
Please see full Prescribing Information, including Boxed Warning, for ARISTADA INITIO and ARISTADA.